Erythropoietin Fails to Improve Visual Outcomes in Optic Neuritis
Erythropoietin added to methylprednisolone did not improve structural or functional outcomes in visual pathways after optic neuritis, the phase III TONE trial found.
Mean 26-week peripapillary retinal nerve fiber layer (pRNFL) atrophy, a structural measure, was 15.93 μm for erythropoietin add-on and 14.65 μm for placebo add-on (adjusted mean treatment difference 1.02 μm, 95% CI –5.51 to 7.55; P=0.76), reported Wolf Lagrèze, MD, of the University of Freiburg in Germany, and co-authors, in Lancet Neurology.
Mean low contrast letter acuity score, a functional measure, was 49.60 for erythropoietin and 49.06 for placebo (adjusted mean treatment difference –4.03, 95% CI –13.06 to 5.01).
“We obtained clear results indicating that erythropoietin confers neither structural nor functional benefits in the visual system,” Lagrèze and colleagues wrote. “Treatment estimates did not approach clinically relevant effect sizes, were not statistically significant, and do not support the notion of erythropoietin as a neuroprotective agent in the visual system.”
“Based on the available evidence, erythropoietin cannot be recommended as an adjunct to methylprednisolone pulse therapy with the aim of improving visual outcomes in optic neuritis,” they added.
The human cytokine erythropoietin has shown neuroprotection in animal models but has produced mixed results in phase II trials of people with optic neuritis. “To our knowledge, TONE is the first sufficiently powered trial to assess the effects of erythropoietin in optic neuritis and the largest in the field of optic neuritis neuroprotection,” Lagrèze and co-authors wrote.
TONE included participants ages 18 to 50 within 10 days of onset of unilateral optic neuritis with visual acuity of 0.5 or less. Overall, 108 patients were enrolled between November 2014 and October 2017. Participants had a mean age of 30; women made up 73% of the erythropoietin group and 65% of the placebo group. No participant had a prior diagnosis of multiple sclerosis, and all were considered to have unilateral optic neuritis as a clinically isolated syndrome. All received methylprednisolone, 1,000 mg per day, intravenously and were randomized either to three days of add-on erythropoietin 33,000 IU or add-on placebo.
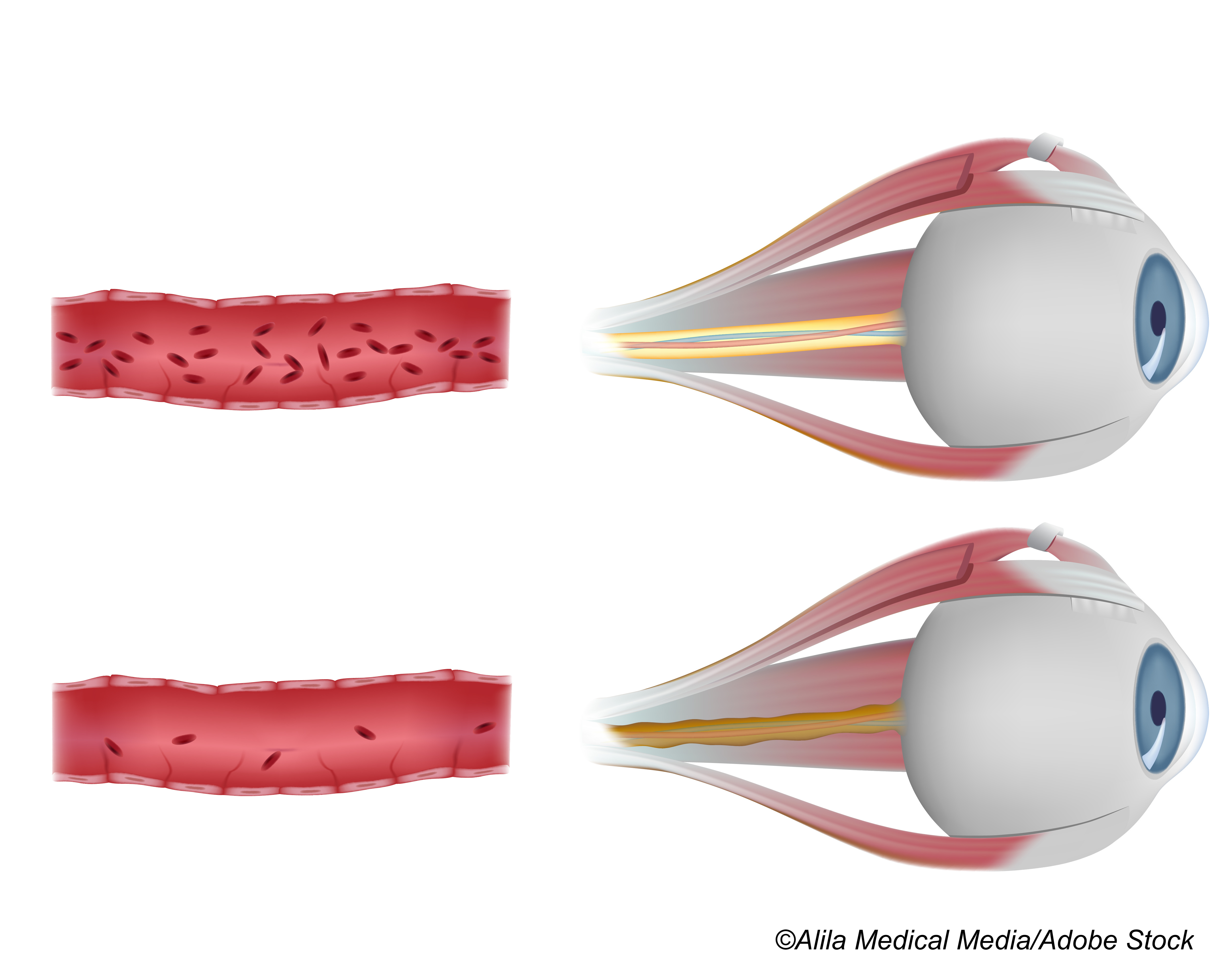
The primary analysis included 52 patients in the erythropoietin group and 51 in the placebo group. Primary outcomes at 26 weeks were atrophy of pRNFL (measured with optic coherence tomography as the difference in pRNFL thickness between the affected eye at week 26 and the unaffected eye at baseline) and low contrast letter acuity.
Adverse events occurred in 81% in both erythropoietin and placebo groups. Headache was most common (25% and 28%, respectively) with other adverse effects of nasopharyngitis (21% and 17%, respectively) and fatigue (13% and 10%, respectively).
Serious adverse events occurred in 15% of the erythropoietin group and 8% of the placebo group. One patient in the erythropoietin group developed venous sinus thrombosis, was treated with anticoagulants and had no sequelae.
At 26 weeks, clinical disability scores in both groups indicated no disability. However, there were conversions to multiple sclerosis: the 26-week multiple sclerosis-free rate for the erythropoietin group was 64% and for placebo 43% (HR 1.91, 95% CI 1.06-3.44).
“All of the secondary outcomes of this trial were negative, with the exception of a difference in multiple sclerosis diagnosis-free survival favoring the erythropoietin group,” Lagrèze and colleagues noted.
“Although studies with disease-modifying medication have shown the possibility of prolonging multiple sclerosis-free survival in patients with clinically isolated syndrome, we believe that our finding should be interpreted cautiously owing to our study design,” they added.
“It could be explained partly by an imbalance in participants unknowingly having multiple sclerosis at trial entry, because the survival curves separate within the first few weeks, during which multiple sclerosis diagnostic work-up is usually completed,” the researchers wrote. “The clinical merits of erythropoietin as a monotherapy for optic neuritis remain unclear. Any future trials of erythropoietin monotherapy would need to address the concern of depriving patients of methylprednisolone, which is still a standard of care in many national guidelines.”
In an accompanying editorial, Fiona Costello, MD, of the University of Calgary, Canada, noted that the TONE study “calls into question the role of methylprednisolone therapy for typical optic neuritis.”
“High-dose corticosteroids provide modest benefits in hastening visual recovery, but they do not affect long-term visual outcomes for patients with typical optic neuritis,” Costello observed.
“Therefore, concerns raised by the authors about depriving patients of methylprednisolone are more likely to reflect practice preference than scientific evidence,” she wrote. “Because approximately 50% of patients with optic neuritis experience at least mild adverse effects caused by high-dose corticosteroids, the questionable advantages of treatment for typical optic neuritis should be acknowledged in patient-informed decision-making models of care.”
Other subtypes of optic neuritis like that associated with MOG antibody-associated disease might have other indications for steroid therapy (e.g., to prevent relapses and protect vision), Costello added. “Differences in therapeutic outcomes highlight the need for robust serological and radiological classification of optic neuritis subtypes, which often have overlapping clinical profiles in the acute setting.”
However, “a clear signal from the TONE study is the need for researchers to be aware of severe thromboembolic complications as a potential risk with erythropoietin use, even in a relatively young study population,” she added.
A 2012 phase II trial of erythropoietin in optic neuritis with 21 people randomized to erythropoietin and 19 to placebo reported decreased thickness in retinal nerve fiber layer thickness at 16 weeks of median 7.5 μm for the erythropoietin group and 29.18 μm for placebo. With other results, the authors concluded there were trends toward an improved outcome after erythropoietin treatment.
A 2019 pilot study of erythropoietin added to methylprednisolone for retrobulbar optic neuritis gave erythropoietin intravenously 20,000 units daily for three days and did not significantly improve 3-month visual acuity, visual field, or contrast sensitivity versus steroid alone. Pace of recovery was also similar between the add-on and steroid-only groups.
In the TONE trial, limitations included an unknown rate of asymptomatic disease activity before study inclusion. This may underestimate pRNFL atrophy as the comparator eye may be less robust, Lagrèze and co-authors acknowledged.
-
Erythropoietin added to methylprednisolone did not improve structural or functional outcomes in visual pathways after optic neuritis, the phase III TONE trial found.
-
Treatment estimates did not approach clinically relevant effect sizes, were not statistically significant, and did not support the notion of erythropoietin as a neuroprotective agent in the visual system, the researchers reported.
Paul Smyth, MD, Contributing Writer, BreakingMED™
This study was funded by the German Federal Ministry of Education and Research.
Lagrèze reported grants from the German Federal Ministry for Education and Research and the German Research Foundation. He received speakers’ honoraria from and worked on advisory boards for Alcon, Allergan, Santhera, Boehringer Ingelheim, and Merz Pharma.
Costello has received speaker fees or advisory board consultant honoraria from Roche, Alexion, Accure Therapeutics, and the Sumaira Foundation.
Cat ID: 130
Topic ID: 82,130,730,130,192,925,240
source https://www.physiciansweekly.com/erythropoietin-fails-to-improve-visual-outcomes-in-optic-neuritis/
Comments
Post a Comment